
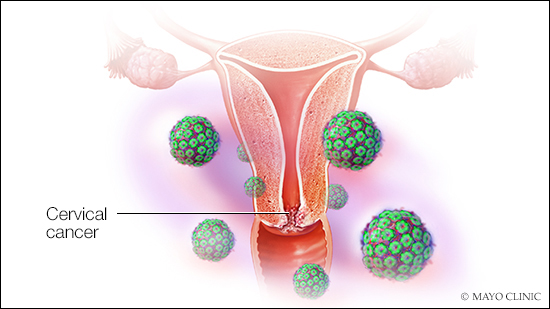
Human papillomavirus (HPV) is the most common cause of cervical cancer. And during January, Cervical Health Awareness Month, women are encouraged to receive the HPV vaccine. They also are encouraged to schedule a screening (pap smear and HPV test) that can find precancerous conditions of the cervix.
HPV infection and early cervical cancer don’t cause noticeable symptoms, so regular screenings can detect changes in the cervix that might lead to cancer in the future. Dr. Chris DeStephano, a minimally invasive gynecologic surgeon at Mayo Clinic in Florida says, “Routine screening every three years with a Pap test or every five years with a pap-HPV co-test ensures precancerous changes are caught early and may be followed more closely or treated.”
The percentage of women who are screened for cervical cancer in the United States ranges between 72-86% based on national data in the United States, but these percentages may be far lower in certain states and racial groups than national data suggests, according to a Mayo Clinic study published in the Journal of Women’s Health. Less than two-thirds of women ages 30 to 65 were up-to-date with cervical cancer screenings in 2016. The percentage was even lower for women ages 21 to 29, with just over half current on screenings.
Dr. Kathy MacLaughlin, a Mayo Clinic family medicine specialist and the study’s lead author, says “African-American women were 50 percent less likely to be up-to-date on cervical cancer screening than white woman in 2016. Asian women were nearly 30 percent less likely than white women to be current on screening. These racial disparities are especially concerning.”
Dr. Olivia Cardenas-Trowers, a Mayo Clinic urogynecologic surgeon and women’s health clinician in Florida says addressing barriers to health care is key, so that all women, including Black women, receive regular routine screening. Screening helps identify cancer early, which leads to better outcomes.
An important limitation raised by Dr. DeStephano is that the pap/HPV test only screens for cervical cancer. Cancers affecting the uterus and ovaries do not have a screening test and are typically identified based on symptoms including vaginal bleeding after menopause and abdominal symptoms including bloating, feeling full when eating, and pressure in the pelvis. It is therefore important to be seen by a healthcare provider every year to discuss recommendations for screening and the development of new symptoms. Virtual visits now provide women more options to discuss symptoms and screening guidelines.

Be the first to comment